I see a lot of patients with digestive complaints; some with heart burn, others with bloating and indigestion and still others dealing with chronic constipation or loose stool.
Insufficient stomach acid production is an often overlooked condition in many people complaining of digestive issues. Instead of finding the root cause, symptoms are addressed with band-aid treatments. If you have heartburn, you are prescribed an antacid (which further lowers your stomach acid levels). If you have IBS this is treated with fiber, laxatives and sometimes an antidepressant. If you have SIBO you are treated with an antibiotic. If you have food sensitivities, you are told to remove this food…. but none of these Band-Aids fix the root cause of the issue. If we look at each of these symptoms and conditions, most of these cases have something in common and that is low stomach acid.
"Reading a great post on Clean & Lean Revolution"
↑ Tweet ThisHeart Burn is Often Caused By Low Acidity
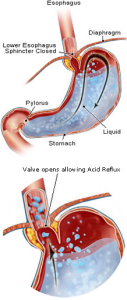
I know that this sounds counterintuitive, but here’s why: If you are not producing sufficient stomach acid then you will not digest your food at a quick enough clip. You need to have adequate stomach acidity to signal the sphincter to close between your stomach and your esophagus. If you don’t have the right stomach pH, then the sphincter won’t close and this will allow the stomach contents to back up into the esophagus, causing heart burn.
 Without sufficient stomach acids, food will not digest well enough. You won’t be able to break food down to the degree that you can access enough nutrition. This sends intact pieces of food into your digestive tract, which can lead to food sensitivities. Yes, removing a known food allergen is a good idea, but, if the underlying condition is not treated, you will likely become sensitive or allergic to another food.
Without sufficient stomach acids, food will not digest well enough. You won’t be able to break food down to the degree that you can access enough nutrition. This sends intact pieces of food into your digestive tract, which can lead to food sensitivities. Yes, removing a known food allergen is a good idea, but, if the underlying condition is not treated, you will likely become sensitive or allergic to another food.
If you aren’t digesting your foods well enough in your stomach, un-digested carbohydrates are fermented by gut flora causing bloating, cramping and sometimes diarrhea and sometimes constipation leading to IBS symptoms. Stomach acids, along with bile acids keep the flora in check at the beginning of the small intestine. When stomach acid is too low, this allows larger levels of flora and other organisms to take up residency in the upper small intestine, leading to SIBO, a small intestinal bacteria overgrowth.
Low stomach acid production has been directly linked to metabolic conditions and even rheumatoid arthritis – when intact pieces of food pass into the blood stream and settle in joints, the immune system can respond by attacking the area around the joints.
Why do some people produce too little stomach acid?
Low stomach acid is linked to hypothyroidism, autoimmune disorders, the use of antacids or proton pump inhibitors, stress, H.pylori, post cancer treatment that includes radiation, it is linked to gastritis – gut inflammation, if you have had gastric bypass you will be at risk. If you have a nutritional deficiency of niacin, zinc or iodine this will all affect stomach acid production.
Let’s get back to talking about the implications of not being able to digest your food. One question I ask in the intake session is ‘do you see any intact pieces of food in your stool.’ This often gets the reply, ‘no, only corn.’ On other occasions, the patient will reply, ‘yes, often.’ Intact pieces of food in your stool, yes, corn and anything else, is a serious symptom. Food is making it through every stage of digestion, un-digested. This may mean that you aren’t chewing well enough, your aren’t producing enough stomach acids or digestive enzymes, it may mean all of these and that there is inflammation or dysbiosis present (an imbalance in gut flora) and it may mean something more serious. As a nutrition detective, it is my job to figure out where the system is breaking down and to help you bring it back into balance.
Should You Supplement?
One of the things that we assess is whether or not you are producing enough stomach acids and whether you may need supplementation or support to produce sufficient stomach acids. A hydrochloric acid or HCL supplement, is an option. When you take this supplement, you aren’t taking enough to change the pH of your stomach. You are simply taking a very small dose that will help to digest the food that it is taken with. It has been shown in studies that taking a hydrochloric acid supplement does not suppress your body’s ability to make HCL. Which is a good thing, because we definitely don’t want to override your body’s ability to produce HCL naturally.
When is HCL Not a Good Idea?
If you have gastritis or an ulcer or a history of these – HCL is going to be contraindicated. You should always take HCL under the care of a qualified practitioner.
Another option is to take bitters. Bitter herbs help to stimulate the stomach to produce more acid. Bitter melon and gentian tea are two widely used bitters. Herbs are also bitters. I always recommend that at least one fresh herb is added to each meal (whether cilantro to a wrap, basil to a salad or chives and parsley to a stir fry).
The bitter taste gets the salivary glands going. It helps the stomach start secreting juices. The bitterness sends the signal to the brain to get the whole digestive tract—the liver, the pancreas, and the intestines—on the lookout for incoming food. One contributing factor to the epidemic issues that we are seeing with digestion is because we have bred the bitter out of food. But this is a topic for another video.
Angela Pifer, Certified Nutritionist
Work one on one with Seattle Nutritionist Angela through her private practice at www.NutritionNorthwest.com
Enjoying this content? Sign up for updates... It's FREE!
Comments
from 18 people
Do H Pylori protocal. Acid suppression anti microbial therapy. Baking soda boswellia resin. Famotidine bismuth. Good luck.
Max
Hi Chris - if you are having issues with higher fat foods, this is pointing to gallbladder issues. I would also look into stomach acid issues - whether too high, or too low, this can affect gastric emptying and digestive signaling. I would also consider parasites as an issue - they can reside in the gallbladder and upper GI and they can slow down digestion as well. The goal is to look at what is setting up SIBO. Warmly, Angela
Angela Pifer
Hi Angela
I’ve recently tested positive for hydrogen SIBO (having had IBS-C and weight loss for years)and currently treating with diet, oregano oil and berberine. After years of elimination and trial and error I’m convinced my trigger is any food that is high in fat. This seems to build up to a flare up. Do you think this could point to the cause of my SIBO / IBS being low stomach acid? I have supplemented meals with a digestive enzyme with 150mg of betaine HCL but this doesn’t appear to make any noticable difference.
Any advice would be mich appreciated.
Chris
Chris
Hi Amanda,
You likely did not do any lasting damage. Your gut lining heals very quickly. I respectfully didn't see the need to test this twice, but yes, confirmed, you do not need to take HCL. I don't recommend bicarbonate 'therapy.' Once healed, you can take digestive enzymes, make sure you are zinc sufficient (I like the Zinc Challenge drink to test this out), chew your food well and drink water away from your main meals. Relax when you eat, this will help improve digestion as well.
Marshmallow root, DGL, glutamine - these can all aid in healing up the lining of your digestive tract.
You are not producing too much stomach acid now. You overdid with the HCL supplement and now just need to give your body some time to heal.
Warmly
Angela
Angela Pifer
After trying to make my body more alkaline by using sodium bicarbonate (baking soda) 2x/day for a year (I was taking 1/2 tsp. AM and PM), I began suffering intestinal issues. I know this was very stupid and misguided.
I found a functional medicine practitioner. He put me on 2 Zypan (a Standard Process supplement ... very low-dose HCL, 175mg per pill) with each meal, as he suspected that I had low stomach acid and very mild SIBO. I also followed a diet similar to the SCD/Low FODMAPS/FTD. All was well, and I did see improvement.
However, I decided to do the HCL test (as we probably have all read about online), just to be certain I was at the right does of HCL. I began with one HCL cpasule (648mg). I never felt a burning sensation ... but, I did begin to get a sore throat. It didn't dawn on me that this could be due to the HCL, as I experienced no other symptoms. However, I eventually experienced bad heartburn when I got to 6 pills. I never experienced heartburn before in my life ... even with each of my five pregnancies. This lasted some time, even after coming off the HCL. But, I finally began to get better.
About three weeks later, I decided to test this one more time to see if it was the HCL that gave me the problems. With just two days on 1 HCL pill (648 mg) at every meal, it all came back: sore throat, swallowing issues (like food is stuck in my throat), heartburn.
I have been off of ALL HCL supplementation for 4 days. The sore throat is beginning to get better. But, I still have some swallowing issues and heartburn.
But, now, I'm freaking out. I am concerned that I have done damage. Could I have caused LPR? Is it possible to induce these issues with HCL? Any suggestions?
I know both FTD books indicate that GERD/LPR are low-stomach acid issues in most cases. However, I feel like just the opposite is happening to me as a direct result of HCL supplementation. Your thoughts???
HELP!!! I'm full of anxiety.
Amanda
Hi Juliana,
HCL will not affect xifaxan in any way.
Angela
Angela Pifer
Hi, I was wondering if it is safe to take HCL while on a 14 day course treatment of Xifaxan?
Thank you!
Juliana
Hi Ryan,
It means that your mucosal immune system is overactive at this time. The goal then, is to figure out why this is overactive. If SIBO, yeast, parasite, leaky gut, mycotoxins... this needs to be addressed and at the same time supporting the immune system (same protocol as addressing adrenal issues - routine, plenty of sleep, move daily, reduce stress, lower inflammation from various pathways).
Angela
Angela Pifer
WHAT IF SIGA IN INTESTINES IS ELEVATED
RYAN
RYAN
Hi Susan,
Low stomach acid isn't directly going to interfere with SIBO treatment (to the degree that you can't overcome it). It is definitely a risk factor and I would address this, so you can improve your ability to digest and aborb, process protein, B12 metabolism, etc. I am not sure what you have used to treat SIBO, so I would look at changing your protocol until you find one that is more effective (testing this along the way to assess its effectiveness, meaning, how much it knocked down the methane based on parts per million on the breath test). I would look at adrenals, anemia, if your immune system is over-responding/ under-responding, get your Secretory IgA tested (fecal test - this is your immune system response at the mucosal level - if low, this is a risk factor for SIBO).
If you want to test for low stomach acids, the Smart Pill (through a GI doc) or the Heidelberg test will help you assess this. I would also look at B12 levels, homocysteine and methylmalonic acid - and iron. Since you already have one autoimmune condition, I would assess for Pernicious Anemia (also an autoimmune condition) and make sure that you have been assessed properly for celiac (hashimotos and celiac prevalence is high).
Angela
Angela Pifer
I have SIBO C and Hashimoto's and have undergone several treatment protocols for the SIBO. I have not been successful yet and I have never been tested for low stomach acid do you think could be part of the solution for me...how to test???
Susan K
Hi Mai,
Digestzymes or Digestive Enzymes Ultra with HCL are two good ones...
Angela
Angela Pifer
Hi Angela
Thanks for the helpful information. What is the digest enzyme that has HCI in it?
Mai
Forgot to write that my "stool" isn't even brown. It's just the food I am eating. I chew really well. Thank you.
Louise
Hi Loise,
My heart goes out to you. I would look at low stomach acid being only part of the issue here. When in famine, the gut will begin to shut down. For example, anorexia is a risk factor for getting SIBO (by no means was this a choice that you had - simply an example that I am sharing). The migrating motor complex (MMC) will stop working in response to very extreme chronic lack of food. You will likely need to address supplement/ medication support to address your MMC pathway, support gut motility, assess thyroid (to see if this is inhibiting gut function), assess autoimmune (to see if this is affecting Secretory IgA and gut function), assess current stress levels... I would focus on cooked and blended foods (really allowing this to do the chewing for you) so you can improve your nutritional status. I recommend not eating raw vegetables - only cooked. It sounds like you are chewing really well - - continue to chew the blended foods (though this might seem weird, it will help to stimulate digestion), try bitters prior to eating...
I hope these ideas help you!
Angela
Angela Pifer
Hello Angela!
My name is Louise and I live in Sweden and I'm 25 years old. During 2009-2013 I was being held captured, and abused every day. I was not given almost any food during this time and weighed 98 pounds when my family found me. I don't produce ANY Hcl. I just see food in my stool. This has given me multiple health issues, as you can imagine. I think that there are many people out there that might have recovered from eating dissorders that have the same problem. I really just can't digest food. I supplement with Hcl and enzymes but this is not enough. I drink tea on shredded ginger and apple cider vinegar. It has been 1 1/2 year since I started treating stomach acid. There almost are'nt any doctor in Sweden who think that stomach acid is the problem. Thank you so much for your answer, I'm really close to just give up.
Louise
Hi Elizabeth, I am going to say 'yikes!!' here! I would never recommend a liquid HCL betaine. Not only are you worried about your teeth, you should also be worried about the lining of the esophagus, which is not at all used to acid. When I work one on one with patients, if warranted, I have them do an HCL challenge, where we test the need for this out. You can find digestive enzymes that have a little HCL in them, and this may be the baseline for most people.
Without enough HCL digestion, at all levels will be impacted, as well as you'll lack the ability to sterilize the food that you eat, so you will be more prone to gut imbalances. Low HCL is one risk factor for SIBO and a risk factor for SIBO reoccurrence.
If you find that you would like additional support - I do work long distance.
Warmly,
Angela
Angela
Regarding HCl supplements. I have an old-ish nutrition book by Adelle Davis called Let's Get Well. She says that HCl is a crutch - and a good crutch, too. In order to encourage your body produce its own HCl, it has to be able to break down & assimilate certain nutrients, esp. minerals & protein. But if you are low in HCl, you can't do this. Catch-22.
So she would advise her clients to take HCl supplements and in her day (1950s & 60s) it wasn't easy to do; you had to take it in liquid form and be careful with it not getting on your teeth. Alternatively, in that era, you would have to take large numbers of tablets. She also mentioned bitter foods.
She also knew an orthopedic specialist who had all his patients take a gastric juice analysis test. I wonder if the doctors today do this or not.
Adelle Davis is not the final word in nutrition, but I can say for sure it is a primary source that can lead you to more info.
Thank you. I'll bet you have carloads of clients, you seem to know a lot - more than most doctors.
Elizabeth